Keywords Cerebral vasospasm, Colforsin daropate hydrochloride, Intra-arterial infusion, Subarachnoid hemorrhage
Abstract
Introduction Cerebral vasospasm remains a leading cause of mortality and morbidity after aneurysmal subarachnoid hemorrhage. This study evaluated the effectiveness and safety of intra-arterial colforsin daropate hydrochloride infusion for refractory vasospasm.
Methods Twenty-nine consecutive patients with angiographically confirmed vasospasm received intra-arterial Forskolin (Colforsin) daropate therapy in a total of fifty-three procedures. Changes in vessel caliber, cerebral circulation time, and clinical status were recorded before and after treatment.
Results Angiographic dilation was achieved after every procedure; forty-seven infusions produced marked vessel enlargement and six produced mild improvement. Among forty-two treatments for symptomatic vasospasm, thirty-six (eighty-six percent) led to clinical improvement. Cerebral circulation time shortened significantly after infusion. At three-month follow-up nineteen patients (sixty-six percent) showed good recovery or moderate disability. Transient headache and tachycardia were the chief adverse effects; hypotension requiring brief dopamine support occurred in two cases. No neurological or hematological complications were attributable to the drug.
Conclusions Intra-arterial colforsin daropate hydrochloride appears to be an effective and safe option for cerebral vasospasm unresponsive to conventional therapy after subarachnoid hemorrhage. Further prospective studies are warranted.
Introduction
Cerebral vasospasm following aneurysmal subarachnoid hemorrhage is a complex phenomenon that can culminate in delayed ischemic deficits. Despite advances in understanding its pathogenesis, an optimal therapeutic strategy has not been established. Endovascular pharmacological angioplasty offers a practical approach, dilating both proximal and distal arteries with relative technical ease. Colforsin daropate hydrochloride, a water-soluble forskolin derivative, directly activates adenylate cyclase to raise intracellular cyclic AMP, producing positive inotropy and vasodilation. This retrospective study reviews our experience with intra-arterial colforsin daropate infusion for angiographically proven vasospasm.
Materials And Methods
Patient Selection
Medical records of eighty-three patients treated within seventy-two hours of aneurysmal rupture between August 1999 and March 2004 were reviewed. Standard management included triple-H therapy and intravenous fasudil until day fourteen. Twenty-nine patients (twenty-two women, seven men; mean age sixty-two years) with angiographic vasospasm refractory to medical therapy underwent intra-arterial colforsin daropate infusion. Twenty-two had symptomatic vasospasm; seven were asymptomatic but showed high velocities on transcranial Doppler with angiographic confirmation.
IAC Treatment
Colforsin daropate (three milligrams diluted in one hundred milliliters saline) was infused at 0.15 mg per minute through a four-French diagnostic catheter positioned in the cervical internal carotid artery just proximal to the ophthalmic segment. Total dose ranged from 1.8 to 12 mg (mean 4.3 mg). Vital signs and neurostatus were monitored continuously.
Angiographic Assessment
Pretreatment angiograms were graded by two observers as mild (< 25 percent narrowing), moderate (25 – 50 percent), or severe (> 50 percent) using admission studies for baseline. Post-infusion studies were classified as good (vessel calibre improved one grade or more), fair (slight enlargement), or negative (worsening). Discrepancies were resolved by consensus with a blinded third reviewer.
Clinical Evaluation
Neurological examinations were performed at two-hour intervals in the neurosurgical intensive care unit. Clinical improvement was defined as resolution or clear amelioration of the deficit prompting treatment. Long-term outcome was assessed at three months by Glasgow Outcome Scale.
Cerebral Circulation Time
Circulation time was measured as the interval from first contrast appearance above the carotid bifurcation to peak opacification of dural sinuses. Comparisons were made between control hemispheres, pre-infusion, and post-infusion studies.
Statistical Analysis
Continuous variables are presented as mean ± standard deviation. Pairwise comparisons used Wilcoxon signed-rank test; independent samples used Mann–Whitney test. Significance was accepted at p < 0.05.
Results
Changes In Vital Signs
Mean systolic pressure fell from 156 ± 27 to 142 ± 37 mmHg (p = 0.011); diastolic pressure fell from 82 ± 16 to 75 ± 20 mmHg (p = 0.039). Heart rate rose from 89 ± 22 to 110 ± 22 bpm (p = 0.001). Values returned to baseline within fifteen minutes after infusion. Two patients experienced transient systolic pressures near eighty mmHg requiring dopamine.
Angiographic Results
Severe vasospasm was present in thirteen procedures, moderate in thirty-eight, mild in two. Good angiographic dilation occurred in forty-seven injections (eighty-nine percent); fair response occurred in six. No procedure aggravated vasospasm. Sixteen patients received multiple infusions (two to five sessions).
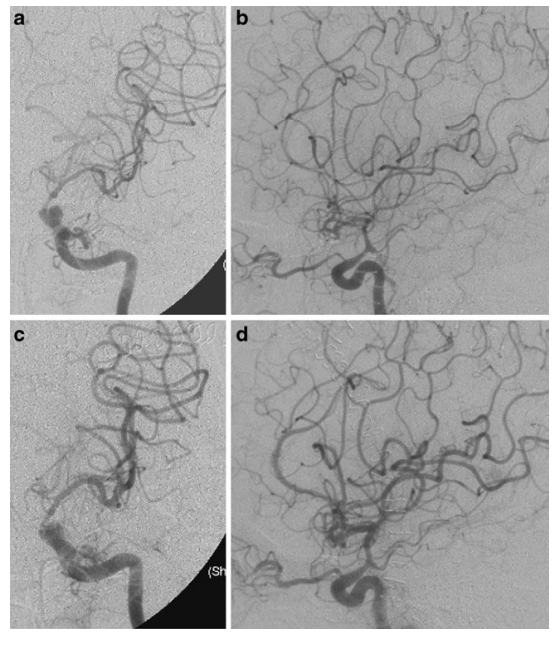
Figure 1. Angiograms from Patient 12.A 42-year-old woman developed gradual onset of aphasia and right-sided weakness (hemiparesis) on day 8 following surgical clipping of an anterior communicating artery aneurysm. Angiograms showed severe vasospasm in the left internal carotid artery (ICA), anterior cerebral artery (ACA), and middle cerebral artery (MCA). Her symptoms improved immediately after receiving intra-arterial colforsin daropate hydrochloride (IAC treatment).a–b: Left carotid angiograms on day 8 showing severe vasospasm in the ICA, ACA, and MCA.c–d: Angiograms after IAC treatment showing significant vessel dilation in both proximal and distal segments.
Clinical Results
Among symptomatic sessions, complete or marked resolution occurred in nine; definite improvement in twenty-seven; no change in six. At three-month follow-up sixteen patients achieved good recovery, three moderate disability, six severe disability, one vegetative survival, and three deaths (one vasospasm-related, two other causes). Computed tomography demonstrated cerebral infarction in seven of twenty-six evaluable patients.
Cerebral Circulation Time
Control hemispheres showed mean circulation time 7.4 ± 0.7 seconds. Pre-treatment vasospasm prolonged time to 8.8 ± 1.7 seconds (p = 0.0012). Post-infusion values shortened to 7.9 ± 1.5 seconds (p = 0.0070 versus pre-treatment).
Adverse Effects
Headache during infusion was common but transient; mild sedation with propofol provided relief. No increases in intracranial pressure, cerebral edema, or hemorrhage were detected radiologically. Laboratory parameters remained stable.
Discussion
Pharmacological angioplasty provides an attractive option for distal and proximal vasospasm. Papaverine, once widely used, poses neurotoxicity and limited efficacy; alternative agents are needed. Fasudil and calcium channel blockers have been explored, but colforsin daropate offers distinct advantages. By directly stimulating adenylate cyclase, it raises cyclic AMP, inducing smooth-muscle relaxation and attenuating calcium sensitivity—mechanisms potentially superior to voltage-channel blockade alone. In this series, intra-arterial colforsin daropate produced immediate angiographic and clinical benefits with acceptable transient systemic effects. Outcomes compared favorably with historical controls despite inclusion of patients with more severe initial grades. Limitations include retrospective design, small sample size, and absence of a control group. Prospective randomized trials are required to define optimal dosing, duration, and comparative efficacy against other vasodilators.
Conclusions
Intra-arterial colforsin daropate hydrochloride achieved rapid and sustained arterial dilation, improved cerebral circulation, and yielded favorable clinical outcomes with minimal complications in patients with refractory vasospasm after subarachnoid hemorrhage. These findings support its consideration as an alternative pharmacological angioplasty agent, pending confirmation in larger controlled studies.